Payment Intelligence®
Find and fix the source of claims processing issues for optimal return on investment.
Leverage a highly configurable tech solution that meets your specific business requirements and helps improve claims operations by addressing the root cause of issues and reducing the noise in your process.
Results: Enhanced savings while paying claims efficiently and effectively.
100+
Health Plans consulting experience leveraged.
4-9%
Up to 4%
120+
Health plans advised.
4-9%
Up to 4%
First year savings through recovery and fixes.
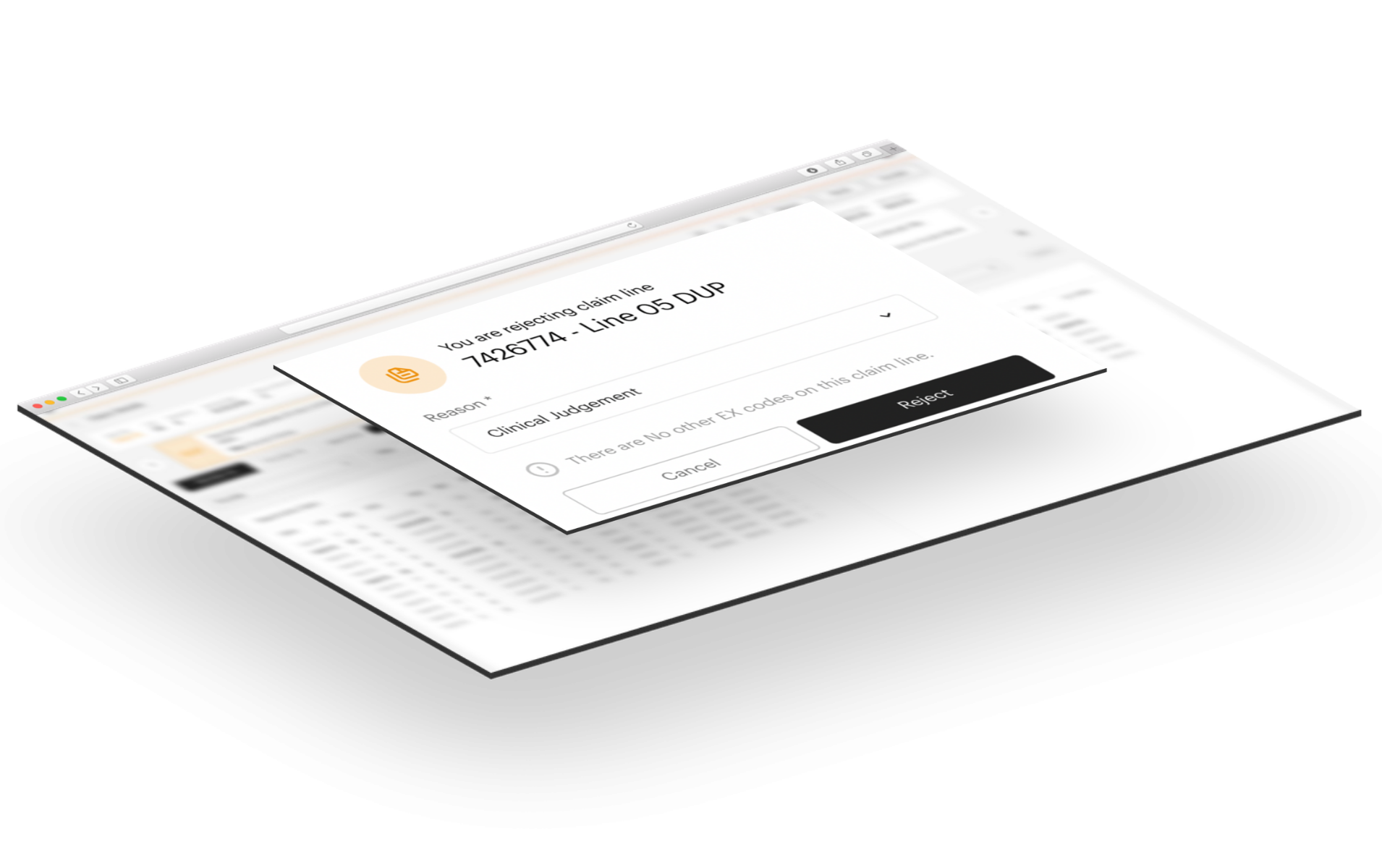
Modern technology infused with healthcare payer expertise
As a health plan, claims need to be paid accurately based on a complex set of contractual and regulatory requirements that go beyond traditional payment integrity. AArete’s Payment Intelligence® provides you with a tool that has been built based on our vast experience helping organizations like yours. By combining that experience with machine learning and artificial intelligence, you get results that reflect your sophisticated needs and adapt to new requirements in this evolving industry.
Increase capacity without more headcount
Planning to grow your membership or provider network? Payment Intelligence® can support the added volume and complexity in claims with intelligence, speed and accuracy in evaluation, while effectively minimizing false positives and appeals.


Be up and running in 90 days
Payment Intelligence® is configured for your needs and processing opportunities in as little as ninety days. See the results reflected is the Ida™ workbench dashboard from the onset.
Find and fix the root cause of costly issues
Post-pay recoupment is a costly process. With our root cause analysis, we identify the source of the problem and help your process become smarter and more efficient, saving you both time and money.

Events
The Future is Now: Embracing Technology and Analytics in your Healthcare Operations Modernization Journey